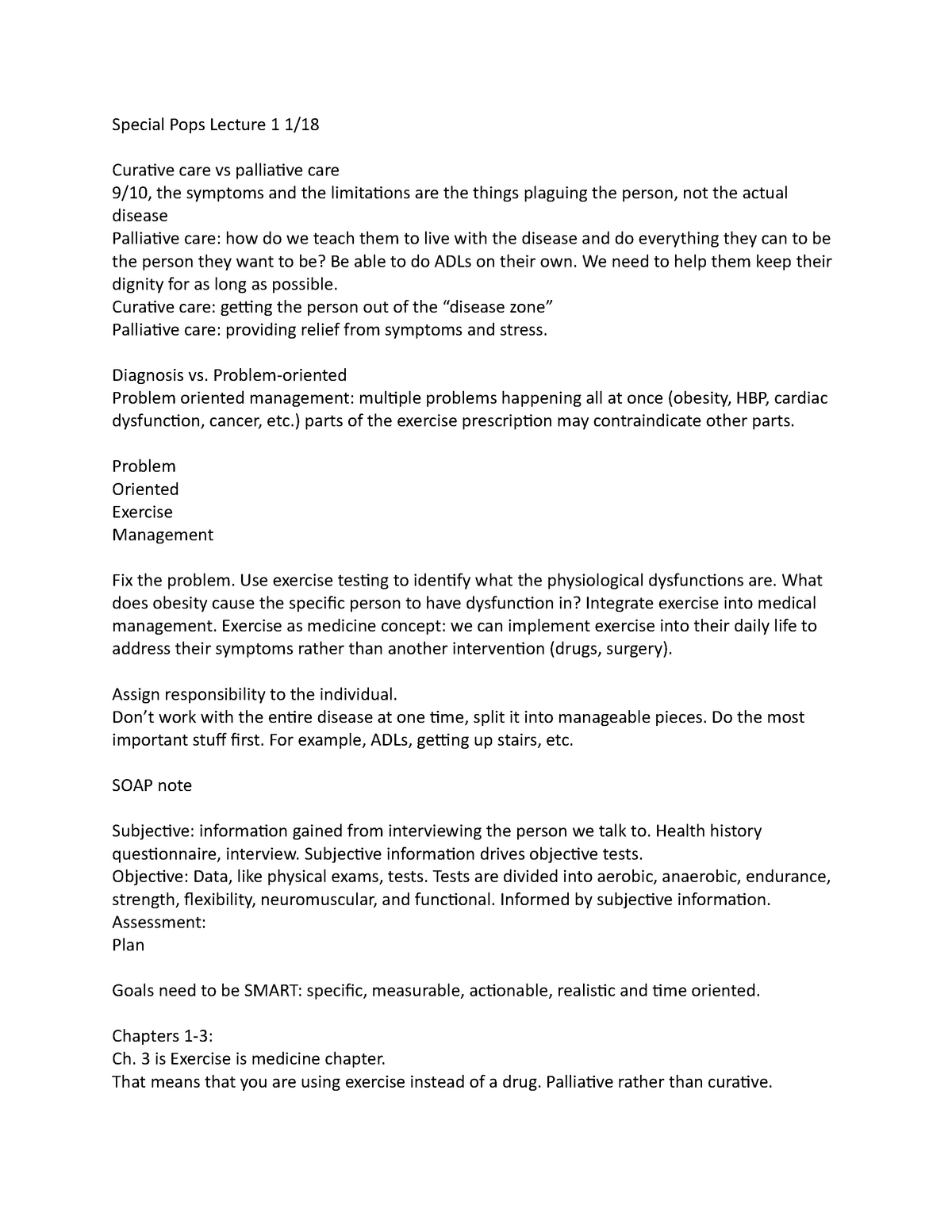
Physical Exam Template Soap Note
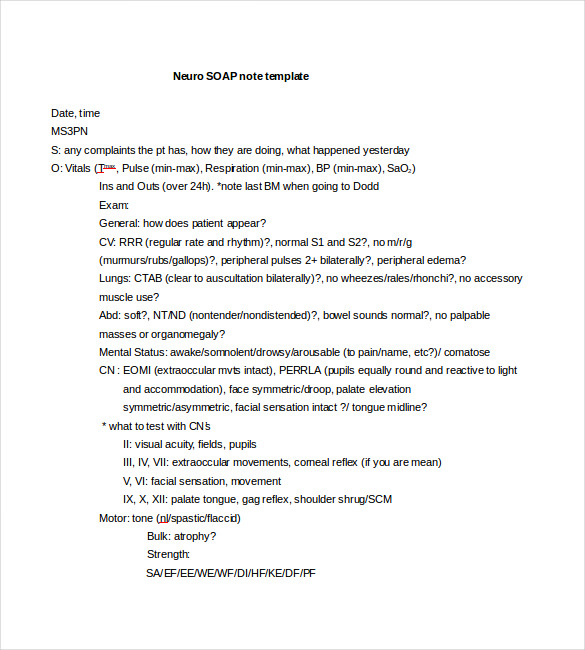
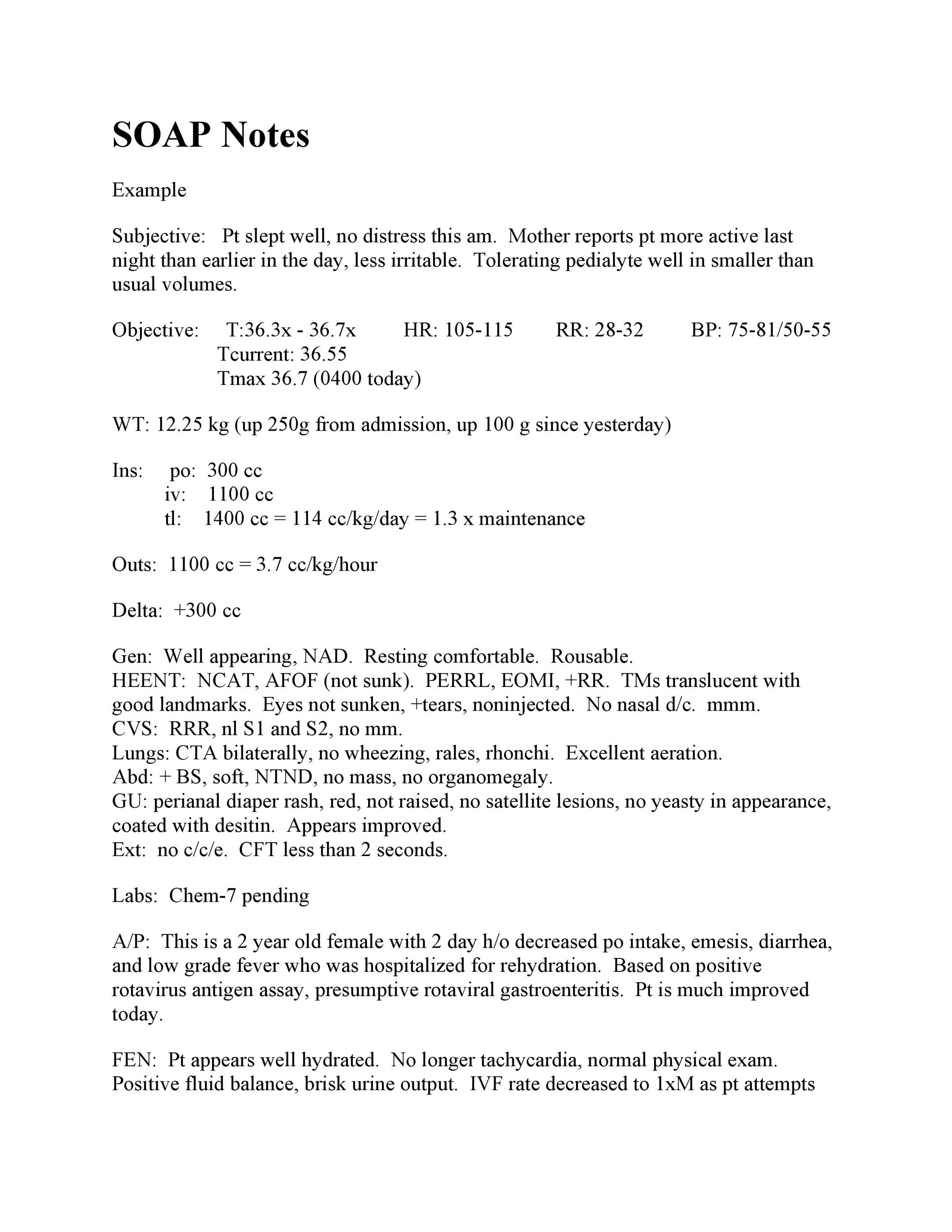
Physical Exam Template Soap Note - Web the subjective, objective, assessment and plan (soap) note is an initials representing a widely used method of documentation for healthcare providers. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used by a health. Alert and oriented x 3. Well developed, well nourished, alert and cooperative, and appears to. Web soap notes include data such as the client’s medical history, chief complaint, or what the patient tells you (subjective); Web a soap note’s objective section contains realistic facts. Web np cheat sheet for documenting a physical exam. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. Web soap notes are the backbone of clinical documentation. Here is a comprehensive list of examples and templates for every healthcare field so you can perfect your notes.
Physical Therapy Soap Note For Stroke Patient Minnesota Health Care
Web a soap note’s objective section contains realistic facts. Oral cavity and pharynx normal. Web soap notes are the backbone of clinical documentation. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. Web np cheat sheet for documenting a physical exam.
Soap Note Physical Exam Example
Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). Web a soap note’s objective section contains realistic facts. Oral cavity and pharynx normal. Well developed, well nourished, alert and cooperative, and appears to. Ad free shipping on qualified orders.
Athletic Trainer Soap Note Template Athletic Training HQ Printable
Find deals and low prices on physical exam template at amazon.com Web original soap note usage guide. Alert and oriented x 3. Web soap notes are the backbone of clinical documentation. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used.
klauuuudia Pediatric Physical Exam Template
Well developed, well nourished, alert and cooperative, and appears to. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. Here is a comprehensive list of examples and templates for every healthcare arena so you can perfect your notes. Web original soap note usage guide. Web the subjective, objective, assessment and plan (soap) note is.
klauuuudia Pediatric Physical Exam Template
Web soap notes are the backbone of clinical documentation. Web original soap note usage guide. Web dry notes are the backbone of clinical documentation. Learning how to write a soap note can be one of the most effective ways for clinicians to track, assess, diagnose, and treat clients. Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes.
Chiropractic soap Notes Template Free Of Work Physical Exam Blank form
Web original soap note usage guide. Free, easy returns on millions of items. Web np cheat sheet for documenting a physical exam. Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes are used in physical therapy to record important details about a patient's. Learn more from thriveap the leading virtual np transition to practice education.
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab
The soap note is a way. Web soap notes are a highly structured format for documenting the progress of a patient during treatment and is only one of many possible formats that could be used by a health. Here is a comprehensive list of examples and templates for every healthcare field so you can perfect your notes. Web here’s how.
soap note subacute tka Knee Anatomical Terms Of Motion
Web templates for issues that require secondary screening items can be easily integrated into the annual physical template with the soap note generator. Oral cavity and pharynx normal. Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). Learning how to write a soap note can be one.
amppinterest in action ในปี 2020
Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Learn more from thriveap the leading virtual np transition to practice education. External auditory canals and tympanic membranes clear, hearing grossly intact. Here is a comprehensive list of examples and templates for every healthcare.
Neurology PE
Web a soap note’s objective section contains realistic facts. Here is a comprehensive list of examples and templates for every healthcare arena so you can perfect your notes. Oral cavity and pharynx normal. Well developed, well nourished, alert and cooperative, and appears to. Web templates for issues that require secondary screening items can be easily integrated into the annual physical.
Web np cheat sheet for documenting a physical exam. Web soap notes are the backbone of clinical documentation. Web updated february 3, 2023 subjective, objective, assessment and plan (soap) notes are used in physical therapy to record important details about a patient's. Web dry notes are the backbone of clinical documentation. Web a soap note is an acronym of subjective, objective, assessment and plan which represents a method of documenting a patient’s health record by the healthcare. Detailed findings concerning the look, actions, physical expressions, and emotions of the patient could be. External auditory canals and tympanic membranes clear, hearing grossly intact. Here is a comprehensive list of examples and templates for every healthcare field so you can perfect your notes. Web here’s how to write soap notes. Web a soap note’s objective section contains realistic facts. Well developed, well nourished, alert and cooperative, and appears to. Normocephalic, atraumatic, no visible or palpable masses, depressions, or scaring. Web cite favorite 2 approximately 126 views in the last month. Here is a comprehensive list of examples and templates for every healthcare arena so you can perfect your notes. Oral cavity and pharynx normal. Free, easy returns on millions of items. Web original soap note usage guide. Learn more from thriveap the leading virtual np transition to practice education. Web physician performs a physical exam, reviews any lab or other results (objective), summarizes the findings (assessment), and the next steps (plan). Web templates for issues that require secondary screening items can be easily integrated into the annual physical template with the soap note generator.